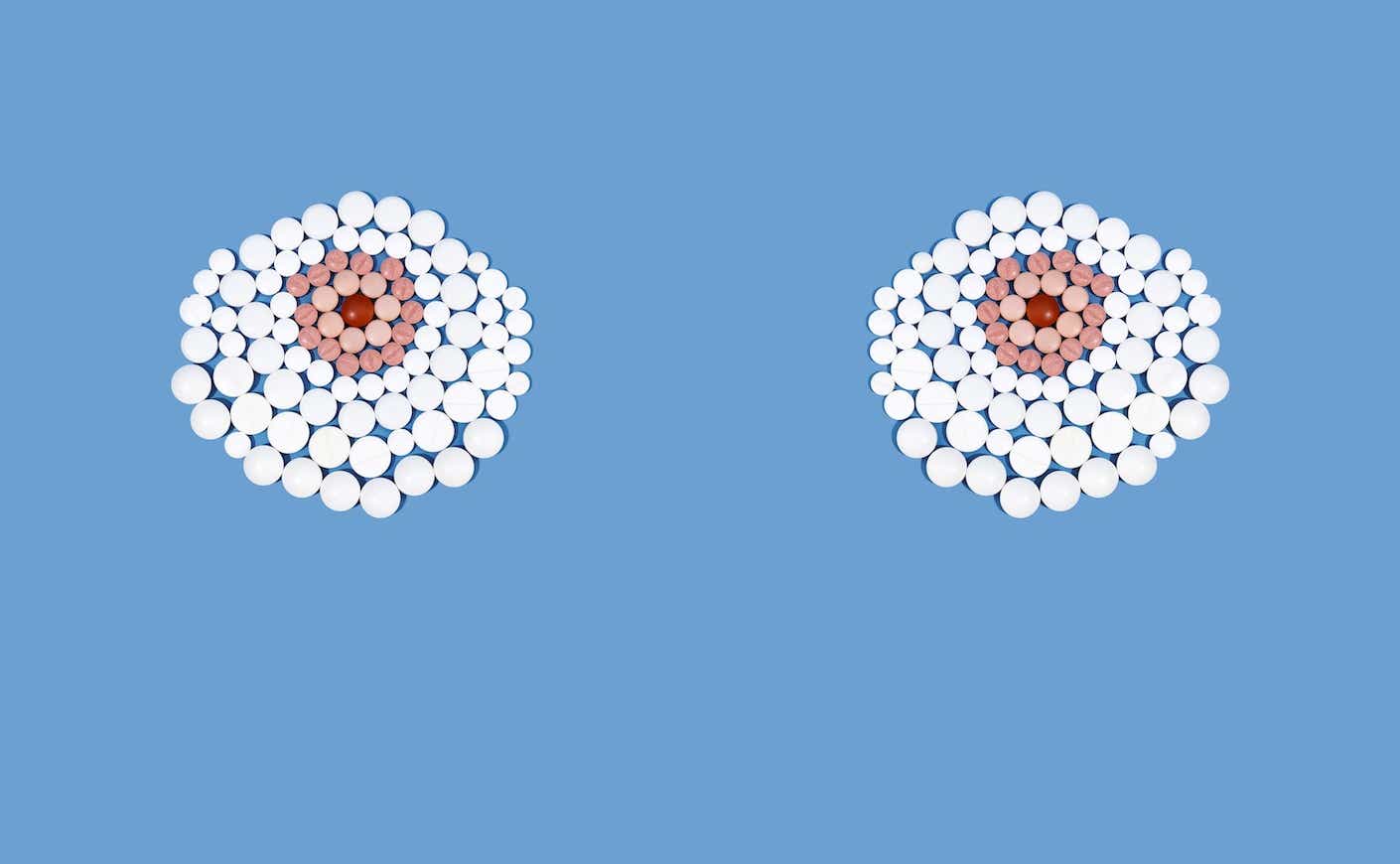
And how they’re used to treat breast cancer.
If you’re diagnosed with hormone receptor-positive breast cancer, like I was in the summer of 2022, you’ve probably learned a lot about AI — but not the AI that’s expected to disrupt virtually every industry — the AI that feels like it’s disrupting your body. I’m talking about aromatase inhibitors — anastrozole, letrozole, and exemestane — drugs that suppress your body’s estrogen production and help prevent cancer recurrence. These are most often prescribed to postmenopausal breast cancer patients because, after menopause, the ovaries relinquish their role as the primary contributors to estrogen production. (Younger breast cancer patients would be prescribed tamoxifen.)
The side effects can be a bummer — so much so that they often make women stop taking them. I wish there was more support for women who are on them, so as part of Breast Cancer Awareness Month, I decided to talk to Patricia Ganz, MD, director of cancer prevention and control research at the UCLA Jonsson Comprehensive Cancer Center. Dr. Ganz helped me understand more about these pesky yet powerful pills. In the end, you’ll probably agree that these symptoms are reasonable trade-offs for the greater benefit of curbing cancer progression.
Katie Couric: I’ve been on aromatase inhibitors for about a year now. And I’m not going to lie, I don’t love them. I was on the estrogen patch for menopause before my breast cancer diagnosis and I MISS MY ESTROGEN! It’s a wonder hormone. Before we talk about living without it, why is estrogen so important?
Dr. Ganz: Estrogen makes a woman a woman. From early in utero, it affects the brain and development of various organs. Estrogen receptors are in almost all organs of the body and during a woman’s reproductive life there are high and cyclic levels that influence many organs. Estrogen is anti-inflammatory, but can also be a source of increased autoimmune inflammatory conditions.
Men also have estrogen, but that’s the product of testosterone, which is really not produced in any quantity until puberty. Their levels of estrogen are considerably lower, but stable throughout life.
So when women go through menopause and estrogen levels drop from about 100-200 units to less than 25 units, they notice the difference in their skin, mood, joints, and vaginal tissue. This low level is in general more troublesome for lean women who do not make as much estrogen in the body after menopause. When the ovaries stop working (average age 51), estrogen in a woman’s body comes from the conversion of male hormones to estrogen. This occurs in the fat tissue. Lean women who have less fat, in general, have lower postmenopausal estrogen levels. They are more symptomatic with hot flashes, sleep disturbance, and vaginal symptoms. But there’s huge variability in these symptoms, and some women have very few symptoms or they may be short-lived. Some women are extremely symptomatic for a long time.
A lot of women with hormone-positive breast cancer are on these drugs. What are you hearing from them?
The majority of breast cancer patients have hormone receptor-positive breast cancers, which are stimulated to grow when they’re exposed to the naturally occurring estrogen in a woman’s body (pre or postmenopausal), and this is then the target for our anti-cancer endocrine treatments. We have two groups of endocrine treatments:
- Tamoxifen, which is a selective estrogen receptor modulator (SERM) that blocks the uptake of estrogen that is circulating in the body from getting into the cancer cell, where it would stimulate growth. This drug works in both pre and postmenopausal women (those with both high and lower estrogen levels) because it prevents the estrogen from getting into the cell. This drug causes hot flashes, sometimes mood changes, and a risk of uterine cancer. But it’s good for the bones and cholesterol. This was the mainstay of endocrine treatment until about 20 years ago when we started using aromatase inhibitors.
- Aromatase inhibitors (three kinds: letrozole, exemestane, and anastrozole) all work by lowering the estrogen level in a woman’s body to near 0 units, taking the level from about 20-25 down to 0. For women who are already having some symptoms of menopause at the level of 20-25, going down to 0 can cause an increase in symptoms, such as hot flashes, joint/muscle pains, and vaginal dryness most commonly. However, again, some women have few symptoms. Usually, those who have menopause symptoms to start with, such as after stopping menopausal hormone therapy (the patch you were on), will have a lot more difficulty because they are going from a level of 75+ units with the patch down to 0 units.
My side effects include muscle and joint stiffness but sometimes I think it’s from pickleball! I just feel much creakier. Is this common? And why is it happening?
This is one of the most common symptoms and really reflects the fact that there are also estrogen receptors in the joints, and they are complaining about the low estrogen levels! Actually, mid-life joint pains start in women in their 40s as the perimenopausal change occurs and for most women, these symptoms increase in their 50s and 60s. In a study I did for breast cancer prevention with tamoxifen and placebo in the 1990s, we saw this pattern of increase in the healthy placebo-treated women. Vaginal dryness also increases during this time and is worse in women in their 60s.
Simply put, aromatase inhibitors exacerbate what’s considered a normal pattern of symptoms in most healthy postmenopausal women.
We’re all wired differently, but joint stiffness is definitely a common problem.
I’m a bit worried about my bones — I did a bone density test and my bones are hanging in, with slight arthritis and some osteopenia which at 66, is sort of normal. (Yay!) What should I be doing to make sure my bones stay strong?
These are good results, and as you say, are normal for your age. Starting at the age of 35, we all start to lose our peak bone mass. There are, of course, contributing factors. If a woman didn’t eat a healthy diet when she was younger, she could have a lower bone mass, and in some patient populations, there is a hereditary component. If there’s an avoidance of sunlight (in northern parts of the world), there could be vitamin D deficiency that affects bone mass.
The best way to maintain bone health is to be physically active and have adequate calcium and vitamin D in the diet.
Should I be taking calcium? And I put collagen in my smoothies. Does that help or is it just a waste of money?
Taking calcium is only necessary if you don’t get adequate intake with your diet. I don’t think there is any evidence that collagen is helpful.
Can we talk about dryness? I’m like the Sahara, Dr. Ganz. I got an Estring and that’s helping a lot. What else can you recommend?
This is caused by the low estrogen effects on the lining of the vagina. There are also vaginal moisturizers that can help, which you apply twice a week. and there are vaginal lubricants to use at the time of intercourse. The New York Times just had a piece on this!
What about the rest of your skin? Are you just going to tell me to moisturize?
Yes, unfortunately, that’s about the best you can do without getting into cosmetic procedures. There are estrogen receptors in the skin as in the vagina and the loss of estrogen is the problem.
I’m also getting a few hot flashes, which I guess is normal. Talk about a blast from the past!
Well, hopefully, they’re not too bad! Several drugs can help if a woman is really troubled, like low doses of some antidepressants (paroxetine and Effexor) as well as gabapentin.
I take my aromatase inhibitor at night. I heard they can cause sleeplessness in some people. Is that true?
I don’t think so. Once you’ve been taking it daily, you have a steady blood level, and the time of day should not make a difference. But often people associate certain side effects with an external event, so they switch and if they feel better will change their pattern.
Any other advice you’d like to give us AI Queens?
I think discussing your symptoms regularly with your doctor is the most important advice I can give because many of these side effects can be helped, and/or get better with time. Sticking with the treatment can be lifesaving and the benefit goes up with larger tumors and those that may have spread to the lymph nodes. There is a 50 percent reduction in the risk of recurrence with five years of treatment, which is very large! Also, changing from one AI to another will sometimes help in managing symptoms, and many doctors use that strategy in our patients.