As you probably know, we lose bone density as we age. And while there's no magic formula to return our skeletons to their former states, there are lifestyle changes you can make to support your bones. Want to know where to start? Katie quizzed her oncology dietician, Emily Buchholtz, RD, CDN, CSO about all things osteopenia and osteoporosis. Buchholtz has previously given us stellar advice on eating to reduce the chance of colon cancer and the truth about supplements. So it makes sense that Buchholtz would be the perfect resource to answer Katie's burning questions about all things bone health and overall wellness. For more on how to keep your bones strong, read on...
Katie Couric: What is osteopenia? I have it, but I really want to keep my bones strong as I age.
Osteopenia is a medical condition characterized by a decrease in bone mineral density. Typically, bones impacted by osteopenia are weaker and have a higher risk of fracture when compared to healthy bone density.
Does osteopenia turn into osteoporosis?
Osteopenia is often considered a precursor of osteoporosis — osteopenia can progress to osteoporosis when left untreated.
Should I be taking a calcium supplement?
Calcium supplementation can be beneficial for people with osteopenia and osteoporosis, but it’s important to confirm with your physician and dietitian before starting a calcium supplement. Not all supplements are created equal, and dosing varies from person to person. The average person with osteopenia and osteoporosis needs about 1,200 mg of calcium per day, and these needs can be met with a combination of supplementation and food. In short, calcium is highly variable: It’s important to establish your baseline needs before adding a supplement.
Do I need to take it with vitamin D for better absorption?
Vitamin D is necessary for proper calcium absorption, and it's common to have inadequate vitamin D levels at some point in time, especially if you live in a colder climate. Sun exposure helps vitamin D absorption, but it’s often hard to meet our vitamin D needs through food alone. But here's some great news: It’s super easy for your doctor to test your vitamin D levels to get a baseline, and they or your registered dietitian can recommend a quality supplement to ensure your needs are met.
Are there foods I should be eating that are high in calcium? What are they?
Yes, there are tons: Some of my favorites include Greek yogurt, salmon or sardines, cottage cheese, tofu, almond butter, almonds, almond milk, tahini, white (cannellini) beans, sweet potato, clementines, dried figs, and dark green vegetables such as kale, broccoli, and cooked spinach.
How much of these foods do I need to eat per day?
The average person with osteopenia and osteoporosis needs about 1200 mg of calcium per day. When someone is on a calcium supplement, I often encourage about 3 servings of calcium-rich foods per day. When someone isn't consuming a supplement, I often encourage about 6 servings of calcium-rich foods per day.
Here are some examples of calcium-rich foods and their approximate calcium content per serving:
Greek yogurt (200 mg per serving), salmon or sardines (200-400 mg per serving), cottage cheese (100 mg per serving), tofu (200-400 mg per half-cup serving), almond butter (70 mg per serving), almonds (75-100 mg per ounce), almond milk (400 mg per serving), tahini (280 mg per ounce), white (cannellini) beans (60 mg per serving), sweet potato (50 mg per serving), clementines (20 per whole fruit, and who can eat just one?), dried figs (160 per serving). Then there's dark green vegetables like kale (100-150 mg per cup), broccoli (45-60 mg per cup), and cooked spinach (240 mg per serving).
Can I eat too much calcium?
Yes, it’s possible. While it's not common to consume too much calcium via food, it is possible to consume excess calcium with supplementation.
Consuming excess calcium on a regular basis can cause hypercalcemia, and be just as harmful as not meeting your calcium needs at all. It can also lead to gastrointestinal issues, kidney stones, and it can interfere with the absorption of other essential minerals like iron and zinc. That’s why it’s important to establish a baseline and work with a professional like a registered dietitian to find the right dosage for your needs.
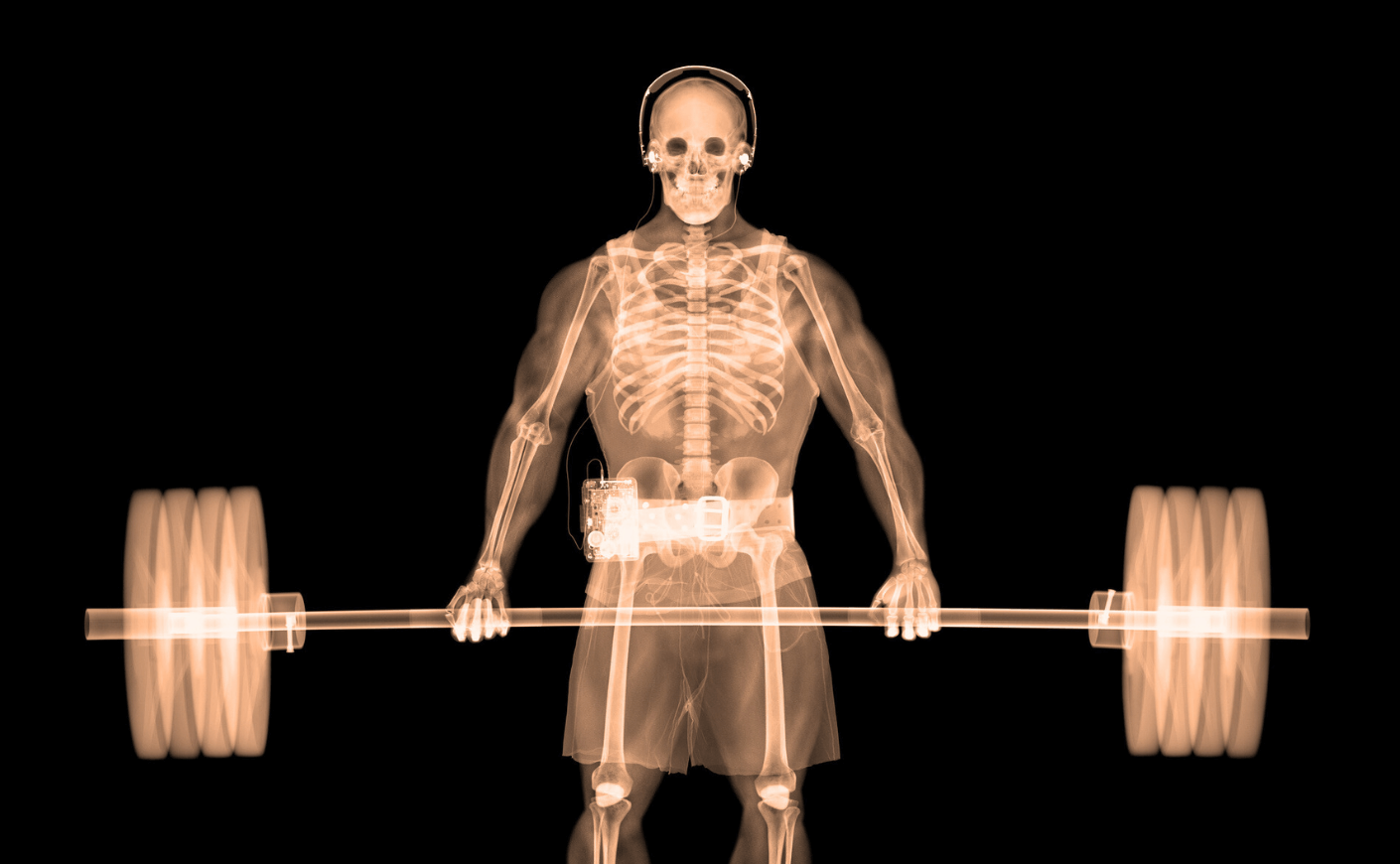
What about exercise? What can I do physically to keep my bones strong?
Exercise plays an important role in managing osteopenia and osteoporosis, by preventing the further loss of bone density. Weight-bearing exercises, resistance exercises, and strength-training exercises are the most effective in supporting bone health — think free weights, resistance bands, weight machines, and bodyweight exercises. If you're a fan of group fitness, HIIT classes, Pilates, and yoga are great options. And if you prefer outdoor exercise, consider power walking, hiking, or jogging; but always check in with your physician before you begin a new exercise routine.