This article is part of an ongoing series providing insights and tips from a primary care doctor on how to get the most from your medical appointments, what your doctor might be experiencing on the other side of the exam table, and all that patients and doctors have in common, so we can make the best of our healthcare system together.
While my clinical colleagues and I rely on the latest scientific data to track waves of Covid-19 infections in our communities, any layperson would be able to tell if there’s a Covid surge just by looking at my inbox. The volume of daily messages from my patients spikes right alongside national infection rates. Whether my patients are worried about how to prevent infection, a recent exposure, managing symptoms of the disease itself, or long Covid, the SARS-CoV-2 virus has led to an undercurrent of anxiety among many of us.
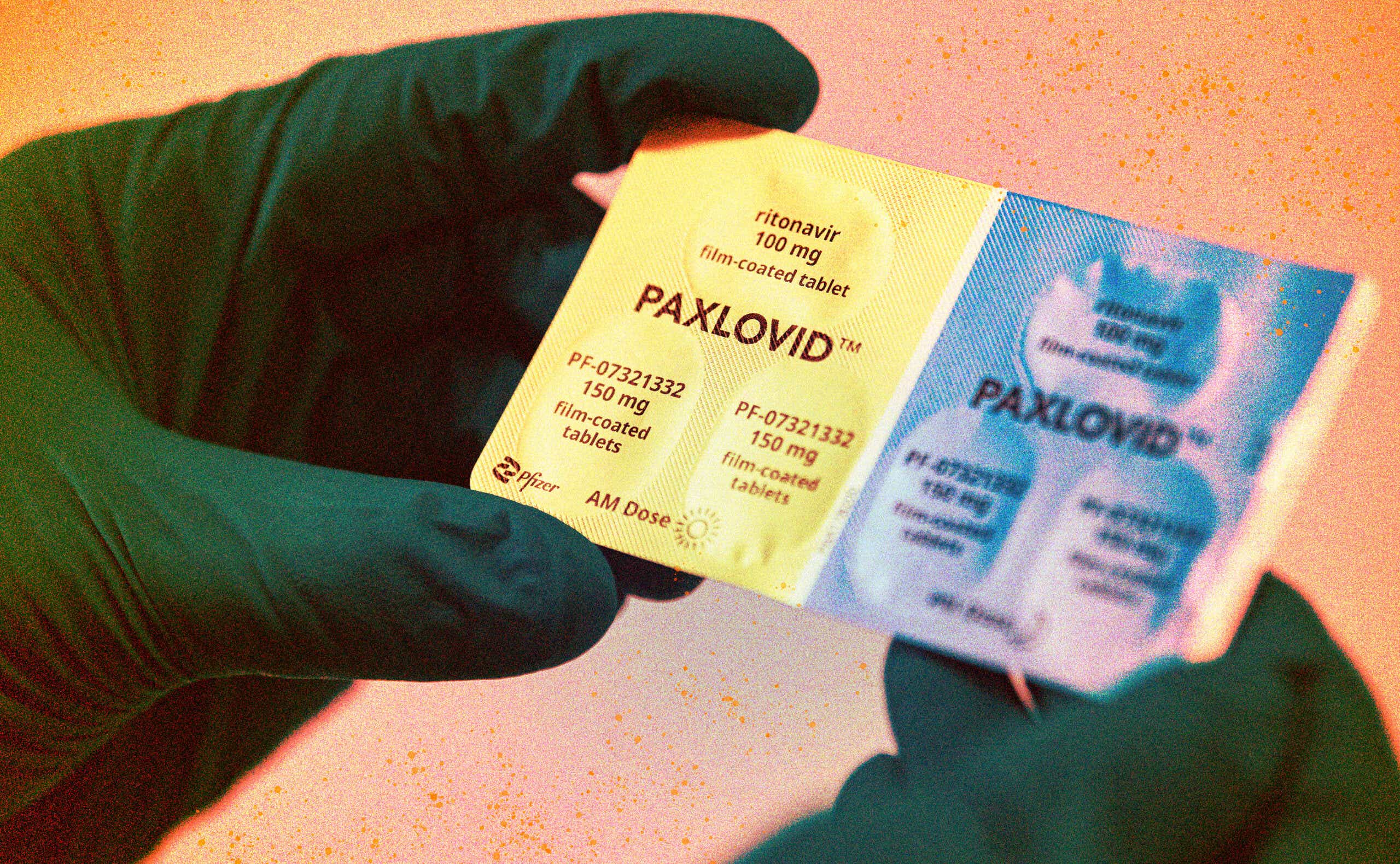
Now, as we experience yet another spike in Covid-19 cases nationally, I admit I’m often surprised by the questions I still receive when it comes to treatment. The main antiviral treatment for Covid-19, Paxlovid (or nirmatrelvir/ritonavir), has been on the market since December 2021, when it was first authorized for emergency use by the Food and Drug Administration. It then received full FDA approval in May 2023.
But Paxlovid is still a mystery to many. I’ve heard from patients confused by who, exactly, should take this medicine, and what factors go into this decision. On the one hand, the drug’s manufacturer, Pfizer, has frequent ads touting, “If it’s Covid, Paxlovid,” prompting some of my patients to ask for the medicine even if it’s not right for them. On the other, national data show that not enough high-risk people are taking Paxlovid when they should.
As an internist, I typically go through the same steps with all my patients as we navigate which, if any, antiviral treatment they should receive. To help you understand your options, I’ve outlined the way I assess the situation with each patient boiled down to the following key questions — three that I ask, and four that my patients ask me.
Questions I ask before prescribing Paxlovid
1. Is my patient a good candidate for Covid-19 antiviral treatment?
Many people should receive antiviral medications when they find out they have Covid, but not everyone. If my patient is young and healthy, then they don’t need anything beyond supportive care — fluids, rest, and over-the-counter remedies to help them feel better.
If, however, they are over the age of 50 or have chronic medical conditions like cancer; chronic kidney, liver, or lung disease; diabetes; or HIV; or if they have undergone organ transplant or are pregnant, then antiviral therapy for Covid-19 makes sense for them. In these cases, either Paxlovid or the other, somewhat lesser-known antiviral treatment for Covid-19 that’s available, molnupiravir, should be prescribed within 5 days of when symptoms started and only if the person has actually tested positive for Covid-19.
While Paxlovid has been shown to be more effective than molnupiravir in preventing serious complications of Covid, including death, it may not be appropriate for everyone. The next questions will help us determine which medication may be best.
2. How are my patient’s kidneys and liver doing?
My first step in determining if Paxlovid is a good option for my patient is to look at their kidney and liver function tests on their most recent blood work. If their kidneys and liver are functioning well, we can proceed to question 3 below.
If they have chronic kidney disease but it’s mild, I can prescribe Paxlovid at a lower dose that’s safer for the kidneys. In severe kidney or liver disease, molnupiravir is likely the safer option as it’s approved for just about everyone other than pregnant or breastfeeding individuals.
3. What other medications are they taking?
Paxlovid interacts with many other drugs in problematic ways. People who take certain medications, like the antiarrhythmic drug amiodarone or phenytoin (Dilantin) for seizure disorder, may not be able to take Paxlovid at all. In these cases, molnupiravir is better because it doesn’t have any known, worrisome drug-drug interactions.
People who take other medicines, like statins for high cholesterol, can take Paxlovid, but they should stop their statins while they’re being treated for Covid-19. The University of Liverpool has a helpful drug interaction checker that I use regularly when advising my patients on how to manage their medications.
Questions my patients ask me about Covid treatment
1. What are the differences between Paxlovid and molnupiravir?
The two medications have many similarities. Both are oral antiviral medications, available by prescription only. Both reduce the risk of hospitalization and death from Covid-19, though Paxlovid tends to be our first choice when possible because of its greater efficacy. Both are taken by mouth twice a day for 5 days. Both should be started within 5 days of when a person starts to feel sick.
There are a few differences, however. Paxlovid is approved for adults and children over the age of 12 and weighing 88+ pounds, while molnupiravir is only approved for adults over the age of 18. Paxlovid has many drug-to-drug interactions that we have to be very careful about researching before we prescribe it. Molnupiravir has minimal drug-to-drug interactions, if any. Paxlovid is safe in pregnancy. Molnupiravir is not.
In my real-world, daily practice, I end up prescribing Paxlovid to most of my patients who need Covid-19 treatment. The times when I prescribe molnupiravir are when my patient is on medications that would have dangerous interactions with Paxlovid.
2. Does my pharmacy have these medications in stock?
Many of my patients would like to pick up their Paxlovid or molnupiravir at their local pharmacy. Not all pharmacies carry these particular medications, though, so I need to check a national Covid-19 therapeutics locator to see where my patient can pick up their prescription. On the whole, more pharmacies have begun carrying these medicines over the past few years.
3. Which side effects should I worry about?
Most people can take these medications without bothersome side effects. The most common side effects of Paxlovid are stomach upset, diarrhea, nausea, and a metallic taste in the mouth. I encourage my patients to take the medication with plenty of water and to stay well hydrated while they take Paxlovid (and while they have Covid in general). Most people can take molnupiravir without many side effects, but diarrhea, nausea, and dizziness have been reported in some patients.
4. Can I get rebound infections after taking Paxlovid or molnupiravir?
Many of my patients ask me about rebound infection after taking Paxlovid in particular. We’re still learning a lot about this phenomenon, which seems to affect between 2 percent and 26 percent of people who take the drug. A more recent review of the literature showed no consistent relationship between treatment with Paxlovid or molnupiravir and rebound symptoms. No matter which study we look at, the majority of people who take these medications do not experience a return of symptoms or a repeat positive test.
If a person does test positive or develop symptoms again after receiving this medication, we recommend supportive treatment — rest, drinking plenty of fluids, and over-the-counter medicines like acetaminophen or ibuprofen to help with fever and muscle aches.
When I go through these questions with my patients who just tested positive for Covid-19, we tend to reach a place of clarity about how they can feel better and hopefully stay out of the hospital. As drained as we all are when it comes to Covid-19, knowing the ins and outs of antiviral treatments can help us get through the next wave of illness, and ensure that people who need treatment the most can use these medications safely.
Neda Frayha, MD, is a primary care internist, editor, and host of the Primary Care Reviews and Perspectives podcast by Hippo Education, and public radio contributor on topics related to health and medicine. She has written for The Washington Post, reported on health care for WHYY, and been featured on podcasts such as The Pulse, The Broad Experience, and The Curbsiders.