Menopause — a natural and inevitable transition for about half the population — shouldn’t be anyone’s cross to bear.
I hadn’t felt like myself lately. Usually an upbeat, productive, friendly person, I felt deflated, flat, lost — as if I’d fallen into a dark hole, unable to climb out and dust myself off. It wasn’t until I’d battled months of sweaty insomnia, a series of mysterious yeast infections which left me clutching a Ziplock of ice cubes on my privates (yes, ice cubes), and a few pubescent-like emotional breakdowns convinced I had no real friends, that I began realizing something was definitely off. I had no idea that this trench that I’d been stuck in was, in fact, perimenopause — or that there was any way to medicate it.
“You’re fine,” one well-respected doctor told me. “It’s just menopause,” he continued casually, eyeing my bloodwork on his clipboard and pointing to the acronym FSH (aka follicle-stimulating hormone), which I later found out was a relatively useless indication of one’s transition into menopause. I left utterly confused, totally caught off-guard, and convinced that my fertility, youth and — in part — my womanhood had been snuffed out like a candle without warning. I was 46.

My beloved OB/GYN, who I’ll call Dr. P, explained to me that I was in perimenopause, not menopause, because I still had my period, although erratic. “Menopause is the moment you’ve gone 12 consecutive months without a period,” she said. At that point, by definition, you’re post-menopausal. Relieved that my ovaries and youth were still present, albeit flickering, I asked how long my seesawing emotions and lack of sleep would last. “It can take months, even years,” she went on, suggesting that I wait until I was period-free before considering any form of hormone treatment. I didn’t push it; I trusted her.
The next year felt like 10. I broke down into tears at my next annual OB/GYN visit, explaining that nothing felt quite right: my body, my emotions, or even my marriage. I’d lost my spark. I used to find joy in my nightly routine — I’d cook dinner with my husband while sharing a glass of wine and talking about our days. Now I found myself snapping at him, annoyed at everyone, including my children, unable to enjoy the things I used to love — wine, a plate of pasta, curling up together to watch a movie. I just wanted to be left alone.
“Is it that bad?” Dr. P asked with a questioning look, her Eastern European accent laced with empathy. “Well…” I shrugged, exhausted. I looked down at the gray linoleum floor and then asked about the hormone treatment that she’d mentioned previously. Was this the wimpy way out? I wondered. Plus, I didn’t believe in excess meds; I barely took Tylenol for a headache. But Dr. P’s opinion was clear: She didn’t recommend HRT, given my mother’s history of breast cancer. Perimenopause was apparently my cross to bear, without the help of any medication.

I kept struggling. The brain fog, lack of sleep, anxiety, and unexplained weight gain continued, further exacerbated by a seemingly disconnected spouse, two hormonal teenagers, and an unsympathetic boss. Even worse, I felt alone, unable to share what I was going through. I found short-term refuge in the healing hands of a talented local acupuncturist focused on female health. She also recommended several nutritional supplements, including golden milk (a calming turmeric drink), maca and black cohort — all of which sparked a much broader rejiggering of my overall nutrition and fitness. (Spoiler alert: Forget the cardio, it’s all about building muscle mass.) I leaned into less-intense, more-consistent strength, mobility, and flexibility workouts, pairing them with mindset and breathwork. I minimized processed foods, inflammatory oils, and excess sugar, and added more protein, fiber, and hydration to my routine. As I grew stronger and more stable, so did my curiosity about overall hormone health.
So I dove into research: hours of podcasts, articles, interviews, and books, all uncovering the complicated truth about the menopause transition, including the devastating role that media had played in denouncing hormone therapy, leaving generations of women to suffer in silence — and the newfound scientific revelations about how hormones really impact a woman’s overall health.
Looking back, I’m so angry: Why didn’t I ask more questions? Why didn’t I have access to more resources? Why didn’t my primary care doctor or OBGYN know more about HRT, including the real risks and broader benefits? The reality is that most doctors aren’t educated about menopause. Some are even biased, based on outdated information. Those who are open to prescribing HRT and accept insurance typically only have 15 minutes to explain it to their patients (good luck with that).
Now 52, I’ve learned that menopause — a natural and inevitable transition for about half the population — shouldn’t be anyone’s cross to bear. No one should have to feel alone as they deal with the myriad menopausal symptoms that can leave women doubting their sanity. And for many, menopause coincides with other, often overwhelming midlife transitions: from changing family dynamics, caring for aging parents, evolving friendships, issues around financial security, and the big question of what’s next?
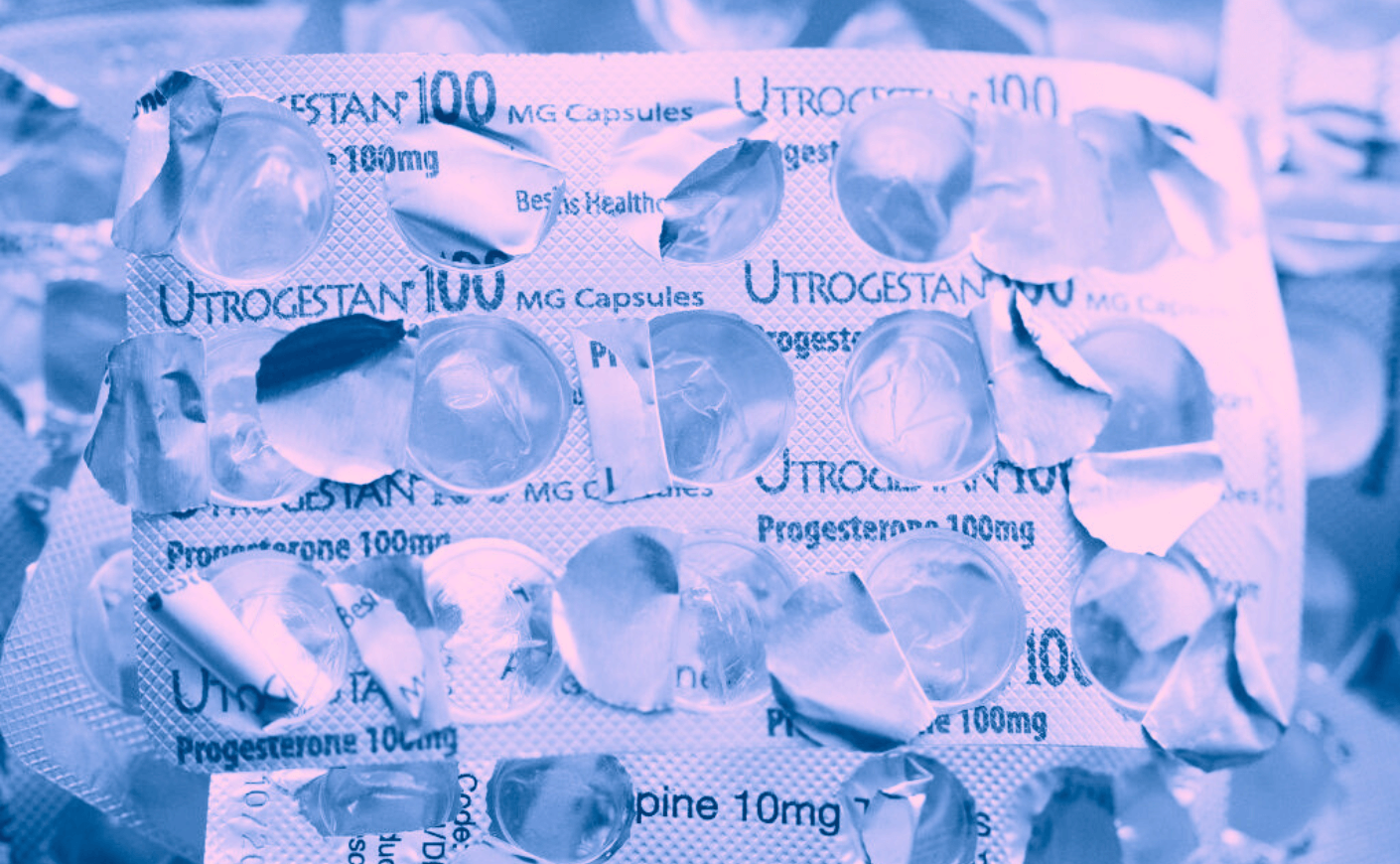
Eventually I found a new doctor, one specializing in integrative medicine and female health. She helped me further connect the dots, from family history, stress levels, and alcohol intake to bone-density scores and risk assessments. She was calm, thorough and informative (but not surprisingly, also out of my insurance network). That doctor prescribed HRT, including transdermal estrogen and oral progesterone, and within weeks, I was sleeping through the night. I felt less edgy, more grounded. Even my long-lost libido showed up to say hello.
What saved me was changing my lifestyle, and finding a knowledgeable doctor — but also learning to advocate for myself. Turns out, I didn’t just have to quietly suffer.
Here’s what I wish I’d known about hormone replacement therapy when I started going through perimenopause.
1. Timing matters
According to Dr. Taz, author of The Hormone Shift and expert on hormonal health, all women can benefit from hormone replacement therapy when needed — and it’s never too early or too late to start. Today’s science and research suggests that HRT can benefit women even pre-menopause. Our ovaries are much more than a reproductive organ; they’re the central command center of our entire female body. They produce a symphony of 54 hormones that help regulate, among other things, our cardiovascular, endocrine, and neurological systems. So there’s a tremendous benefit to keeping our ovaries working for as long as possible, and supplementing with HRT as they begin to decline. And if you missed the boat on taking them during perimenopause, HRT can have long-term health benefits for women when it’s started up to 10 years after menopause.
2. HRT is for more than just hot flashes
The best-known reason to consider HRT is to alleviate the symptoms associated with the transition to menopause, most notably fatigue, mood swings, hot flashes, and painful sex. But research is proving that HRT can significantly impact other aspects of a woman’s health and wellness, including bone loss and risk of heart attack. So even if you’re not experiencing debilitating menopause symptoms, it’s worth finding out if HRT is an option for you.
3. HRT isn’t as scary as we once thought
There have been decades of hype and fear around the use of HRT, largely due to the media’s misrepresentation of the now-infamous 2002 Women’s Health Initiative (WHI) study, which claimed that HRT led to an increase in breast cancer. This study was deeply flawed on many levels: Most notably, these trials were designed to determine the benefits and risks of taking HRT for chronic disease prevention, not as a means to alleviate menopause symptoms. In addition, Dr. Taz notes that the estrogen these women were given was Premarin, which is synthesized from horse urine and doesn’t biochemically or structurally resemble the estrogen that women naturally produce. As a result of these misconceptions, decades of women, including myself, suffered in silence with no significant options for treatment.
4. You have way more treatment options than you think
Believe it or not, most doctors aren’t educated on how to treat menopause: According to AARP, only 20% of OB/GYN residencies offer menopause training, and half of all U.S. OB/GYN medical residents felt they needed more education on menopause medicine. So be sure to find a doctor who’s experienced in this field and understands the treatment options, including non-hormonal options, and can help you assess the risk/benefit of each.
Also, consider finding a doctor who no longer delivers babies — assuming you’re not in the market for one — as they’re more likely to be focused on female health in midlife and beyond. And remember, like most treatments, HRT isn’t a panacea. “There’s no quick fix,” says Dr. Taz, who takes an Eastern-meets-Western medicine approach, providing patients with a deeper understanding of how any prescribed hormones affects the rest of the body, particularly your liver and gut. She emphasizes that our long-term health and wellness is also tied to overall lifestyle, including fitness and movement, nutrition, and mindfulness.
5. You’re not alone
Dollars to donuts, many women around you are experiencing the same cocktail of confusion, fear, anxiety, and even shame. So reach out to your network. Be intentional about building a tribe of not only health and wellness professionals, but also friends who you can talk to during this transitional time of your life — even if that means being open to new pals. Find the people you can be open and honest with, because aging means facing even more pivotal moments of change and transition. And you’ll be able to face them together.
* Talk to a trusted medical professional to learn more about what nutritional supplements and other medical treatments that may be right for you.
Julie Flakstad is a writer | speaker | and founder of The Midlife Truth Project. Follow her @julieflakstad and learn more at julieflakstad.com.








