I vow to love you in sickness and in health. It’s a phrase that anyone who’s attended a wedding or seen a rom-com knows by heart. They’re words that mark the beginning of a couple’s married life, though not necessarily a sentiment that most people give a lot of thought to when making a lifelong commitment. But what if your healthy partner suddenly becomes sick, and your future together becomes complicated? When Daria Kaliman was just 35 years old, the vow she’d taken eight years prior — “in sickness and in health” — suddenly became real.
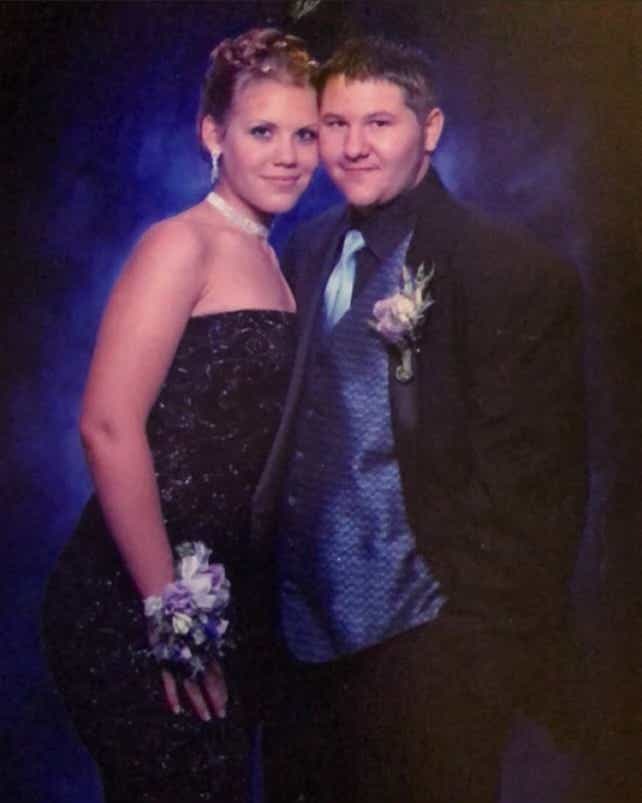
Kaliman met her husband Justin in high school in Lakeview Terrace, CA, when the two were only 14. “He was shy, and I’m an extrovert, so I was intrigued,” remembers Kaliman. “But he was very cute, and he turned out to be really funny and sweet, too.” The pair bonded over their shared love of music and clothing, and their friendship quickly turned into a romance.
In 2015, the couple eloped in Las Vegas, and then moved to Pasadena, CA, where they became the proud pet parents of two large dogs and two cats. Justin began working at his family’s courier business while Kaliman attended graduate school to earn a degree in marriage and family therapy. “We settled into day-to-day life,” says Kaliman.
Everything was normal. It was good.
But then one day, Kaliman began noticing some troubling changes in her husband. “He was so tired, and would cancel plans,” she says. “It was like he was sick all the time, and his illness just wouldn’t go away.” As Justin’s symptoms continued to worsen, he finally went to the hospital, where the couple’s worst fears were realized: Justin was diagnosed with diffuse large B-cell lymphoma, or DLBCL, an aggressive form of non-Hodgkin’s lymphoma – a common type of blood cancer. The diagnosis was terrifying, and the couple had some immediate decisions to make about how to help Justin going forward.
“Right after we learned he had cancer, things were awful. It was obviously a stressful time for Justin, but it was a stressful time for me, too,” says Kaliman. “I had a full caseload of clients, and was in my final year of my four-year graduate program. Weighing all of that against what Justin would need was pretty heavy.” While the couple grappled with what this diagnosis would mean for Justin, Kaliman also had to consider how it would change her future.
It almost felt like cancer was this unwanted third person who had joined our marriage.
“I had to ask myself, What can I do to accommodate this in our life?” she says. “I couldn’t let myself even consider the fact that he could die. So I just decided he would get better. I would buckle down, and take care of him, and be present.” She decided to put her education on pause and care for Justin full-time.
“He was in a wheelchair, so I helped him get around everywhere. I would help him bathe and get dressed, and make his meals,” says Kaliman. At times, she felt the need to detach from her feelings in order to care for Justin: “I had worked at residential and intensive outpatient treatment centers, so I’m pretty good in a crisis,” she says.
Sometimes I would have to lean into my training and ask myself, How would I handle this situation if this wasn’t my husband? If this were one of my patients, how would I approach this?
Becoming a full-time caregiver for a loved one is a huge decision, and one that can have serious consequences. From her work, Kaliman was well-aware of the dangers of caregiver burnout, which according to the Cleveland Clinic is “a state of physical, emotional and mental exhaustion that happens while you’re taking care of someone else.”
One of the best ways for caregivers to avoid burnout and its negative mental and physical health impacts is to regularly take time for themselves and avoid hiding their feelings from others. Luckily, Kaliman took steps to protect herself from day one. “I was very lucky,” she says.
I had a wonderful therapist, and she was there for me whenever I needed her. When I would get overwhelmed, she was my lifeline.
Kaliman also wasn’t afraid to lean on others for support: “We had incredible friends and family with us throughout Justin’s treatment. They would make us meals and drop them off, and were always eager to help with anything I needed.”
With this support system in place, Kaliman felt confident in her ability to help make crucial and informed decisions with Justin about his treatment. It was then the couple learned from Justin’s hematologist-oncologist about a treatment called Polivy® (polatuzumab vedotin-piiq), which is combined with other medicines (rituximab, cyclophosphamide, doxorubicin, and prednisone), as a first treatment for adults who have moderate to high risk DLBCL, not otherwise specified or high-grade B-cell lymphoma. With this disease, early treatment is crucial to provide patients with the best chance at remission, given that approximately one in three of those diagnosed may see their cancer relapse or not respond to first-line treatment at all. Along with Justin’s oncology team, Kaliman and Justin decided that this was the right treatment plan for him. He was treated with the Polivy regimen every three weeks for six cycles.

Based on the results of the clinical trial that his hematologist-oncologist participated in as the principal investigator at City of Hope, the Food and Drug Administration approved the Polivy regimen in April 2023 as a treatment for adults with previously untreated DLBCL. All medicines have side effects. In the clinical trial of Polivy, the most common side effects were nerve problems in the arms and legs, nausea, tiredness or lack of energy, diarrhea, constipation, hair loss, and redness and sores of the lining of the mouth, lips, throat, and digestive tract. Call your healthcare provider or get emergency help right away if you develop any signs or symptoms of serious side effects. More important safety information can be found below this article.
After the shock of going from being a perfectly healthy adult to being confined to a wheelchair, too weak to perform even the most basic of daily tasks, Justin began to notice a difference in his blood test results over the course of his treatment. In February of 2024, a follow-up scan was completed and the couple were informed of the positive news. Seven months after being diagnosed, Justin was officially declared to be in remission.* “I saw how Justin was progressing, and I knew the news would be good,” says Kaliman. “And it was.”
In January of this year, Justin felt confident enough in his independence that Kaliman finally felt ready to go back and finish her degree; she graduated in the spring. “Walking across that stage was emotional for me,” says Kaliman.
Given how things could have gone, it was amazing Justin was there to witness that moment. It was a real celebration, which was something we needed.

As they enter this next chapter of their lives, the impact of Justin’s diagnosis is still very present: “We lost our ability to have children, so we’re still processing that,” says Kaliman. “We were gonna wait until I graduated to have kids, and then life kind of made that choice for us. But we still have options, and we’re open to adoption or fostering.” Even with these new obstacles, Kaliman remains an optimist. “We don’t know what’s going to happen, and life is full of unknowns,” she says. “But whatever comes our way, Justin and I are going to handle it together.”
Learn more about Justin’s story, and how Polivy is used as a first treatment for adults who have moderate to high risk diffuse large B-cell lymphoma (DLBCL).
The information in this story is specific to one patient’s experience and is not a substitute for consulting your own doctor. If you have diffuse large B-cell lymphoma, talk to your doctor about your individual symptoms and potential treatment options.
*In a large clinical trial of 879 people newly diagnosed with certain types of large B-cell lymphoma, Polivy plus R-CHP reduced the risk of people’s cancer worsening or returning by 27% compared with traditional chemoimmunotherapy (R-CHOP; a combination of Rituxan, cyclophosphamide, doxorubicin, vincristine and prednisone). There were no differences in response rates.
Polivy U.S. Indication
POLIVY is a prescription medicine used with other medicines (a rituximab product, cyclophosphamide, doxorubicin, and prednisone) as a first treatment for adults who have moderate to high risk diffuse large B-cell lymphoma (DLBCL), not otherwise specified (NOS) or high-grade B-cell lymphoma (HGBL).
Important Safety Information
Possible serious side effects
Everyone reacts differently to POLIVY therapy, so it’s important to know what the side effects are. Some people who have been treated with POLIVY have experienced serious to fatal side effects. Your doctor may stop or adjust your treatment if any serious side effects occur. Be sure to contact your healthcare team if there are any signs of these side effects.
• Nerve problems in your arms and legs: This may happen as early as after your first dose and may worsen with every dose. Your doctor will monitor for signs and symptoms, such as changes in your sense of touch, numbness or tingling in your hands or feet, nerve pain, burning sensation, any muscle weakness, or changes to your walking pattern
• Infusion-related reactions: You may experience fever, chills, rash, breathing problems, low blood pressure, or hives within 24 hours of your infusion
• Low blood cell counts: Treatment with POLIVY can cause severe low blood cell counts. Your doctor will monitor your blood counts throughout treatment with POLIVY
• Infections: If you have a fever of 100.4°F (38°C) or higher, chills, cough, or pain during urination, contact your healthcare team. Your doctor may also give you medication before giving you POLIVY, which may prevent some infections
• Rare and serious brain infections: Your doctor will monitor closely for signs and symptoms of these types of infections. Contact your doctor if you experience confusion, dizziness or loss of balance, trouble talking or walking, or vision changes
• Tumor lysis syndrome: Caused by the fast breakdown of cancer cells. Signs include nausea, vomiting, diarrhea, and lack of energy
• Potential harm to liver: Some signs include tiredness, weight loss, pain in the abdomen, dark urine, and yellowing of your skin or the white part of your eyes. You may be at higher risk if you already had liver problems or you are taking other medication
Side effects seen most often
The most common side effects during treatment were
• Nerve problems in arms and legs
• Nausea
• Tiredness or lack of energy
• Diarrhea
• Constipation
• Hair loss
• Redness and sores of the lining of the mouth, lips, throat, and digestive tract
POLIVY may lower your red or white blood cell counts and increase uric acid levels.
POLIVY may not be for everyone. Talk to your doctor if you are
• Pregnant or think you are pregnant: Data have shown that POLIVY may harm your unborn baby
• Planning to become pregnant: Women should avoid getting pregnant while taking POLIVY. Women should use effective contraception during treatment and for 3 months after their last POLIVY treatment. Men taking POLIVY should use effective contraception during treatment and for 5 months after their last POLIVY treatment
• Breastfeeding: Women should not breastfeed while taking POLIVY and for 2 months after the last dose
These may not be all the side effects. Talk to your healthcare provider for more information about the benefits and risks of POLIVY treatment.
You may report side effects to the FDA at (800) FDA-1088 or http://www.fda.gov/medwatch. You may also report side effects to Genentech at (888) 835-2555.
Please see the full Prescribing Information and visit https://www.POLIVY.com for additional Important Safety Information.









