Between the mood swings, skin issues, and body changes, perimenopause seemingly impacts your every waking moment. But for those of us in the midst of that transitional period, the symptoms don’t stop there — it can interrupt your nights, too. All kinds of sleep issues can rear their ugly head in the run-up to menopause, with a 2023 study finding that more than half of women (51.6%) deal with sleep disorders during the change. And considering the profound effects of lack of sleep, especially in the long-term, this is an issue that you can't afford to ignore.
Nobody wants to spend all night watching the numbers on the clock change, or wake up feeling groggy. So we tapped an expert, Andrea Matsumura, MD — a board-certified sleep medicine physician — to answer our biggest questions about shut-eye.
Katie Couric Media: What kinds of sleep changes or disruptions can happen during menopause and perimenopause?
Dr. Andrea Matsmura: During perimenopause and menopause, many women experience difficulty falling asleep, staying asleep, or waking too early. Hot flashes and night sweats can cause repeated awakenings, and some women notice more-frequent snoring, restless legs, or more fragmented, lighter sleep overall.
Why does that happen?
Menopause doesn’t just affect the ovaries; it rewires the entire brain-body system, and sleep is often the first casualty. Hormonal shifts in a woman’s body change how we get to sleep, and stay asleep. Those shifts involve a drop in estrogen, which disrupts the body's production of progesterone, testosterone, and melatonin — what I call your "sleep squad." Similarly, the decline in progesterone levels also lowers GABA activity, which increases anxiety and restlessness and makes it more difficult to fall asleep.
A decline in testosterone can mean less energy, poorer recovery, and more fragmented sleep. On top of that, decreased melatonin production throws off the circadian rhythm; hot flashes and night sweats can jolt you out of sleep; and general hormonal instability causes cortisol spikes. That stress, in turn, can cause you to wake up early in the morning or contribute to sleep anxiety.
Finally, postmenopausal women also have a higher risk of undiagnosed obstructive sleep apnea.
If a patient comes to you saying, “I can’t sleep like I used to,” which tests or evaluations do you typically recommend?
I start with a detailed sleep and medical history; a review of medications; and screening for conditions like sleep apnea, restless legs syndrome, anxiety, and depression. Basic labs can help rule out thyroid issues, anemia, and other metabolic contributors. If symptoms suggest a primary sleep disorder, I may recommend an overnight sleep study or at-home sleep apnea testing, or start on menopause hormone treatment if indicated.
Which red flags signal that someone's menopausal sleep problems might require a specialist or sleep study?
Certain symptoms definitely warrant further evaluation. They include loud snoring, choking or gasping during sleep, significant daytime sleepiness, morning headaches, uncontrolled restless legs, worsening insomnia despite good sleep habits, or sleep affecting safety — such as avoiding driving due to sleepiness.
Does hormone therapy impact sleep?
Hormone therapy can improve sleep for some women, especially those whose sleep is disrupted by night sweats and hot flashes, as hormone therapy works to lessen these symptoms. It’s not a universal solution, but when used appropriately, it can meaningfully reduce sleep disturbances related to vasomotor symptoms.
Are there any supplements you recommend for sleep?
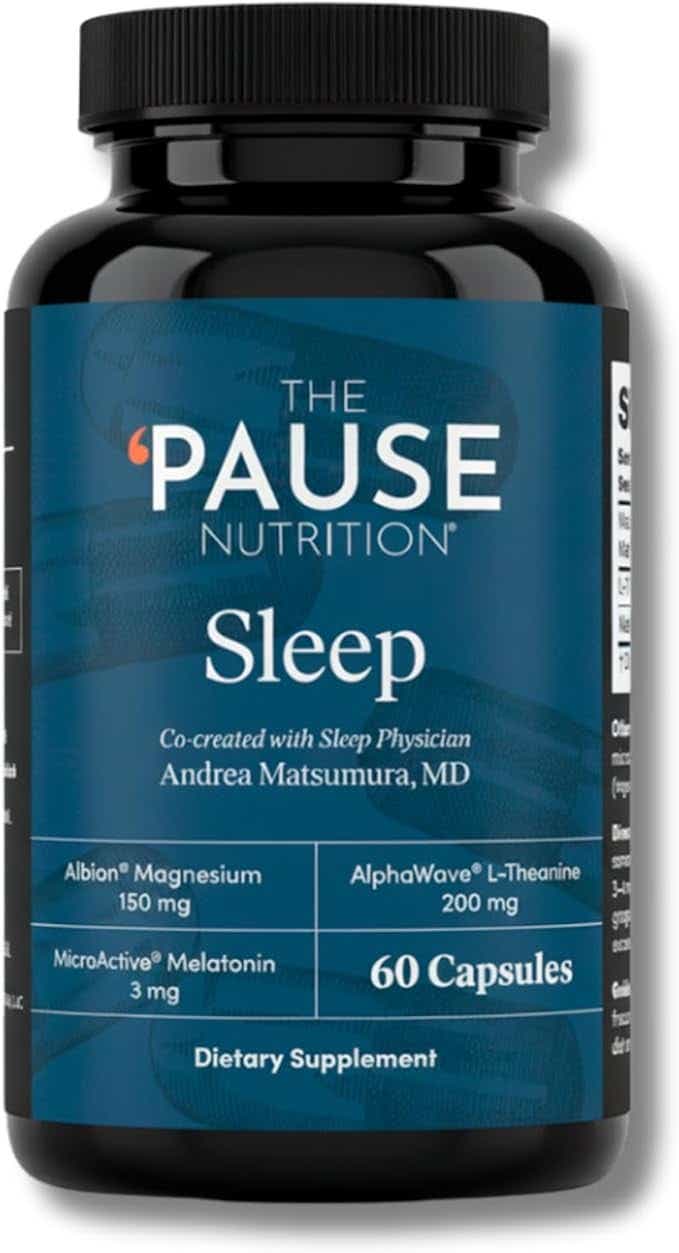
I prioritize behavioral and lifestyle strategies first, but if it's appropriately dosed, melatonin can be helpful. I co-created a sleep supplement with Dr. Mary Claire Haver which contains 3mg of slow-release melatonin, along with L-theanine and magnesium. These are research-backed ingredients proven to support the body in promoting and sustaining sleep. It's not a cure for insomnia, but a support tool for promoting quality sleep.
Poor sleep itself increases cardiovascular risks, so it's important to address. And when used properly, melatonin supports healthy circadian rhythm and sleep quality.
If a woman can only make one change starting tonight, what’s the most impactful thing she can do for better sleep?
Set a consistent wake-up time every day. Consistency anchors your sleep-wake rhythm and naturally improves your ability to fall asleep and stay asleep over time.
Also, if you’re navigating menopause and struggling to sleep, know this: You're not broken. You don't have to “just live with it.” And you're not alone. We need a cultural shift in how we talk about and treat sleep in midlife women. It’s not a luxury. It’s a biological necessity. And it’s time we take it seriously.