Sponsored by GSK.
Dr. Lewin has been compensated by GSK for her participation in this article.
Did you know that the most common type of female reproductive cancer is found in a part of the body many women can’t identify on a diagram?
We’re talking about endometrial cancer, a type of uterine cancer. The American Cancer Society estimates that there will be about 68,000 new cases of uterine cancer in the U.S. in 2024, and national rates are expected to rise about 18 percent between 2022 and 2040. Physicians often use the terms uterine cancer and endometrial cancer interchangeably, since endometrial cancer makes up the overwhelming majority — 90 percent — of uterine cancer cases.
If you’re not sure where your uterus is, you’re not alone — one poll suggests that almost 60 percent of women can’t identify the uterus in a diagram. But it’s never too late to start learning, especially since the United States has the highest rates of endometrial cancer of any developed country. That’s why we asked gynecologic oncologist Sharyn N. Lewin, MD, FACS, to help us understand this part of the body, identify the signs and symptoms of endometrial cancer, and share information about a treatment option for patients with certain types of endometrial cancer.
Understanding your uterus
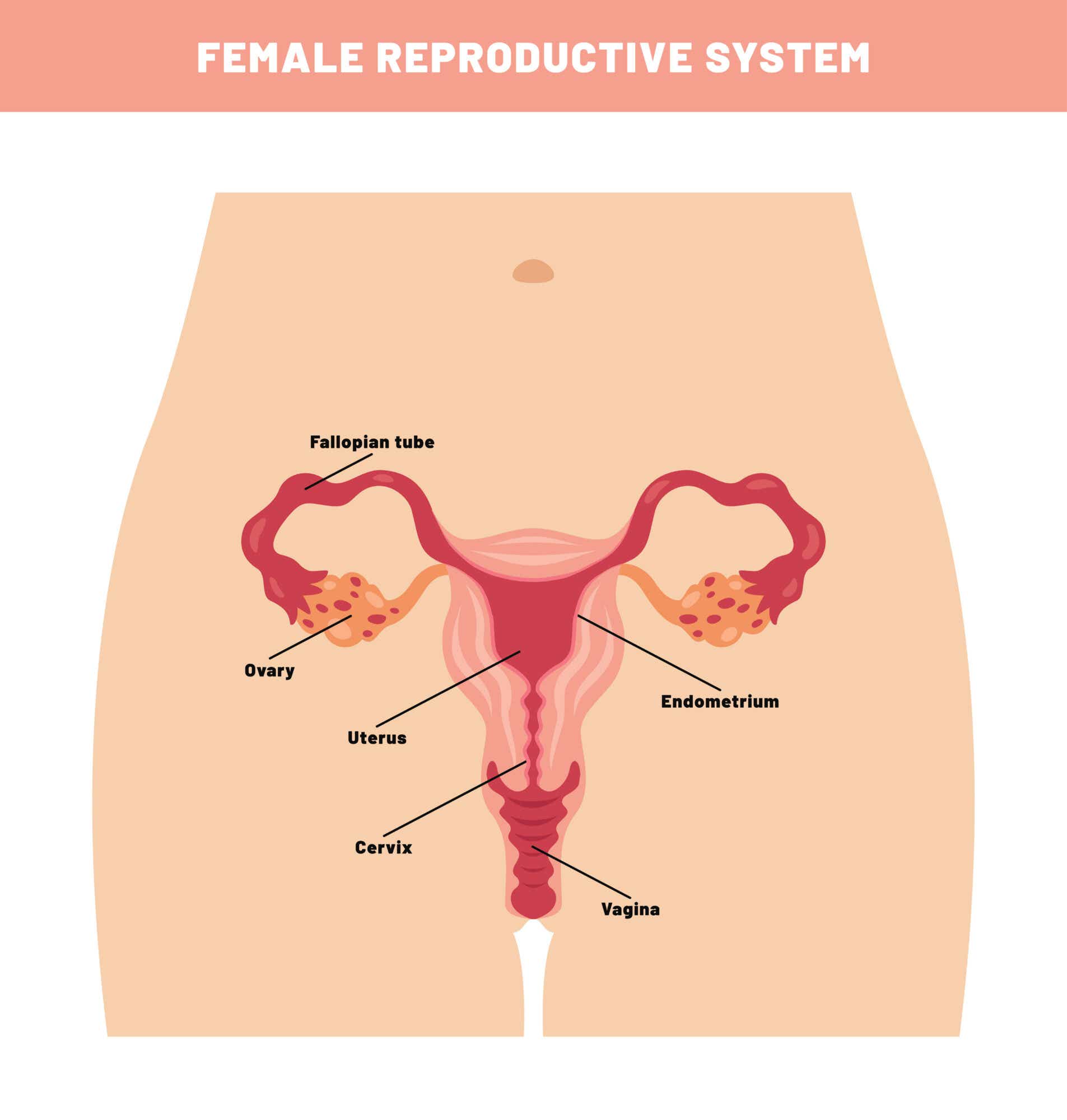
Let’s start with the basics: The female reproductive system has five internal organs. “People often refer to the pelvic organs as the ‘vagina,’ explains Dr. Lewin, “but that’s just one small part of a much larger system.” The vagina leads up to the cervix, which then opens into the uterus. The uterus is located in the pelvis between the bladder and rectum and is supported by the pelvic floor, which includes the muscles that hold up organs near the pelvis, including your bladder. The uterus’s primary function is to grow a fetus during pregnancy. Normally it’s about the size and shape of a pear, but it can expand up to five times its size. Within the uterus is the endometrium, or layer of uterine lining (this is where endometrial cancer forms). The function of the endometrium, or uterine lining, is to thicken each month in anticipation of possible pregnancy. If a fertilized egg is implanted, the lining stays in place to support the pregnancy; if an egg is not implanted, the endometrium thins and sheds as a menstrual period.
“Many women don’t know how our reproductive organs connect because we can’t see them,” says Dr. Lewin. “In general, women in the U.S. tend to have low awareness that certain symptoms such as abnormal vaginal bleeding can be related to gynecologic cancers, and that’s a huge problem. It’s incredible what a uterus can do — it’s where our periods come from and where babies grow, but it’s also where endometrial cancer develops. We need to do a better job in helping women understand their bodies so if a problem arises, they’re aware of what to look out for.”
Who is at risk for endometrial cancer?
Endometrial cancer mainly affects postmenopausal women, with 60 being the average age at diagnosis. Menopause is defined as an entire year without a period, and the time period after going an entire year without a period is referred to as postmenopause.
Some of the risk factors for endometrial cancer include family history, obesity, and things that affect one’s hormone balance, like taking estrogen after menopause. As with many cancers, you may have a higher likelihood of developing gynecologic cancer if it runs in your family, so make sure to learn your family history if possible to better understand your potential risk. While rates for endometrial cancer are steadily increasing for all racial and ethnic groups, Black women see a higher mortality rate than other race groups. This is likely due to several reasons, including that Black women are more likely to be diagnosed with rarer and more aggressive forms of endometrial cancer.
Take spotting seriously
Unlike some cancers, endometrial cancer may have an early warning sign: spotting, which is characterized as light vaginal bleeding. Spotting doesn’t always indicate a serious medical issue, but the timing of the spotting and how long it lasts are important factors that can help determine its cause. In Dr. Lewin’s experience, “Spotting in between periods or change in bleeding after the age of 35 calls for a biopsy.” Any abnormal bleeding, especially after menopause, can be a cause for concern, she says.
Dr. Lewin says once a woman is postmenopausal, bleeding from the vagina should trigger an immediate trip to the gynecologist: “I’ve had postmenopausal patients tell me their period has come back,” she says. “If you’re postmenopausal, any bleeding or spotting is not a period. It is a sign something might be wrong.”
There is no routine screening test for endometrial cancer
Passing reproductive age also doesn’t mean you should skip your regular visit to the gynecologist. “Even after menopause, you should go in for a checkup every year,” says Dr. Lewin. “And if anything looks or feels off, schedule an appointment right away.” Other symptoms of endometrial cancer include lower pelvic pain and unintentional weight loss. But as with any cancer, not all patients will experience all symptoms, so you should talk to your doctor if you notice any of these symptoms or if something feels different than usual.
The assumption might be that when you get a pap smear, you’re getting screened for endometrial cancer. Unfortunately, this isn’t true. “In a pap smear, we screen for cells in the cervix, which is the entry point into the uterus,” says Dr. Lewin.
While there’s no tried-and-true screening method for endometrial cancer, pap tests can sometimes reveal signs of an abnormal endometrium (lining of the uterus), which may prompt follow-up tests to check for endometrial cancer. However, “to detect endometrial cancer, we’ll generally start with an ultrasound to look at the lining of the uterus,” says Dr. Lewin. “If the patient is postmenopausal and her lining looks thick (more than 4mm), that’s a clue there may be an abnormality.” This is followed by a biopsy, where doctors take a sample of the uterine lining to test.
Treating endometrial cancer
If you are diagnosed with endometrial cancer, there are different approaches to treatment based on your age, stage at diagnosis, and family history.
With endometrial cancer, the course of treatment depends on the stage at which a patient is diagnosed. The stage typically isn’t known until surgery is performed. “If a patient has endometrial cancer, the standard approach is to go straight to surgery,” says Dr. Lewin. “We’ll do a full hysterectomy to remove the uterus and cervix, as well as remove the ovaries and fallopian tubes. We often also perform other tests like lymph node mapping to see if the cancer has spread. We may also take imaging on the chest, abdomen, and pelvis to see if there’s any disease outside of the uterus.” Treatment after surgery may include chemotherapy with or without radiation or immunotherapy.
If a patient is diagnosed at a later stage, they will likely need additional treatment. “For the past couple of decades, there was little advancement in newly-diagnosed advanced endometrial cancer care,” explains Dr. Lewin, “so there were limited options for these women. I’m happy to say we now have additional treatment options.”
One such option is JEMPERLI (dostarlimab-gxly for injection 500mg). In August 2024, the U.S. Food and Drug Administration approved JEMPERLI for another use, in combination with chemotherapy medicines carboplatin and paclitaxel, in patients with newly-diagnosed endometrial cancer that has spread outside their uterus (advanced) or has returned. JEMPERLI is a type of immunotherapy, which is a type of drug designed to help immune T-cells — the cells in the body that fight infections — identify and attack tumor cells. Immunotherapy drugs work with the body’s immune system to treat cancer.
Approved Uses
JEMPERLI is a prescription medicine used to treat adults with a kind of uterine cancer called endometrial cancer (EC)
- JEMPERLI may be used in combination with the chemotherapy medicines, carboplatin and paclitaxel, and then after that JEMPERLI may be used alone:
- when your cancer has spread outside your uterus (advanced) or,
- your cancer has returned.
- JEMPERLI may be used alone:
- when a laboratory test shows that your tumor is mismatch repair deficient (dMMR), and
- your cancer has returned, or it has spread (advanced EC), and
- you have received chemotherapy that contains platinum and it did not work or is no longer working, and
- your cancer cannot be treated by surgery or radiation.
It is not known if JEMPERLI is safe and effective in children.
Dr. Lewin ensures that all her patients understand potential side effects when discussing treatment options. Because JEMPERLI is an immunotherapy, it can cause someone’s immune system to attack normal organs and tissues in any area of the body. These problems can become severe or life-threatening and lead to death. More than one of these problems can occur at the same time, which may happen during or after treatment. It is important to call or see a doctor right away for any new or worsening signs or symptoms. Immune system problems can include lung problems, intestinal problems, liver problems, hormone gland problems, kidney problems, skin problems, and problems in other organs and tissues. JEMPERLI can also cause severe or life-threatening infusion reactions, rejection of a transplanted organ, and complications in people who received a bone marrow transplant that uses donor stem cells.
These are not all the potential side effects that can occur with JEMPERLI; please review the Important Safety Information below and the full Prescribing Information, including Medication Guide, to learn more.
“I think immunotherapy approvals are an important step forward for women with advanced or returned endometrial cancer,” says Dr. Lewin.
On a personal level, Dr. Lewin remains hopeful about the progress she’s seen in some of her patients. “I have a patient in her 50s with stage IV (4) endometrial cancer, and she had multiple lung lesions,” says Dr. Lewin. “She’d been having symptoms for a long time, but didn’t recognize them.” While in the past there would have been few options for a patient with this type of advanced endometrial cancer, Dr. Lewin was able to offer her patient another option. After discussing the potential risks and side effects mentioned previously, her patient started JEMPERLI. “While every patient’s experience is different, she responded well to this regimen of carboplatin and paclitaxel in combination with JEMPERLI, and now she’s just on JEMPERLI alone.”
“The goal is always to find this cancer early,” says Dr. Lewin. “But if we do discover it at a later stage, we have another treatment option in our arsenal.”
If you are diagnosed with endometrial cancer, the best first step is to find a great care team — one that will provide both expert guidance through treatment options and emotional support. Understanding diagnosis methods and treatment options may increase the likelihood of a successful outcome, and when you’re in capable hands, you can approach the journey with hope. For more information, talk to your doctor and visit www.jemperli.com.
Important Safety Information
JEMPERLI is a medicine that may treat certain cancers by working with your immune system. JEMPERLI can cause your immune system to attack normal organs and tissues in any area of your body and can affect the way they work. These problems can sometimes become severe or life-threatening and can lead to death. You can have more than one of these problems at the same time. These problems may happen anytime during treatment or even after your treatment has ended.
Call or see your healthcare provider (HCP) right away if you develop any new or worsening signs or symptoms, including:
Lung problems. Signs and symptoms may include cough, shortness of breath, or chest pain.
Intestinal problems. Signs and symptoms may include diarrhea or more bowel movements than usual; stools that are black, tarry, sticky, or have blood or mucus; or severe stomach-area (abdomen) pain or tenderness.
Liver problems. Signs and symptoms may include yellowing of your skin or the whites of your eyes, severe nausea or vomiting, pain on the right side of your stomach area (abdomen), dark urine (tea colored), or bleeding or bruising more easily than usual.
Hormone gland problems. Signs and symptoms may include headaches that will not go away or unusual headaches, eye sensitivity to light, eye problems, rapid heartbeat, increased sweating, extreme tiredness, weight gain or weight loss, feeling more hungry or thirsty than usual, urinating more often than usual, hair loss, feeling cold, constipation, your voice gets deeper, dizziness or fainting, changes in mood or behavior such as decreased sex drive, irritability, or forgetfulness.
Kidney problems. Signs and symptoms may include change in the amount or color of your urine, blood in your urine, swelling in your ankles, or loss of appetite.
Skin problems. Signs and symptoms may include rash; itching; skin blistering or peeling; swollen lymph nodes; painful sores or ulcers in your mouth or in your nose, throat, or genital area; fever or flu-like symptoms.
Problems can also happen in other organs and tissues. These are not all of the signs and symptoms of immune system problems that can happen with JEMPERLI. Call or see your HCP right away for any new or worse signs or symptoms. Signs and symptoms may include chest pain, irregular heartbeat, shortness of breath, swelling of ankles; confusion, sleepiness, memory problems, changes in mood or behavior, stiff neck, balance problems, tingling or numbness of the arms or legs; double vision, blurry vision, sensitivity to light, eye pain, changes in eyesight; persistent or severe muscle pain or weakness, muscle cramps; low red blood cells, bruising.
Infusion reactions that can sometimes be severe or life-threatening. Signs and symptoms of infusion reactions may include chills or shaking, itching or rash, flushing, shortness of breath or wheezing, dizziness, feel like passing out, fever, back or neck pain.
Rejection of a transplanted organ. Your HCP should tell you what signs and symptoms you should report and monitor you, depending on the type of organ transplant that you have had.
Complications, including graft-versus-host-disease (GVHD), in people who have received a bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be serious and can lead to death. These complications may happen if you underwent transplantation either before or after being treated with JEMPERLI. Your HCP will monitor you for these complications.
Getting medical treatment right away may help keep these problems from becoming more serious. Your HCP will check you for these problems during treatment with JEMPERLI and may treat you with corticosteroid or hormone replacement medicines. If you have severe side effects, your HCP may also need to delay or completely stop treatment with JEMPERLI.
Before receiving JEMPERLI, tell your HCP about all of your medical conditions, including immune system problems such as Crohn’s disease, ulcerative colitis, or lupus; received an organ transplant; have received or plan to receive a stem cell transplant that uses donor stem cells (allogeneic); have received radiation treatment to your chest area; have a condition that affects your nervous system, such as myasthenia gravis or Guillain-Barré syndrome.
If you are pregnant or plan to become pregnant, tell your HCP. JEMPERLI can harm your unborn baby. If you are able to become pregnant, your HCP will give you a pregnancy test before you start treatment. Use an effective birth control method during treatment and for 4 months after your last dose of JEMPERLI. Tell your HCP right away if you become pregnant or think you may be pregnant during treatment with JEMPERLI.
If you are breastfeeding or plan to breastfeed, tell your HCP. It is not known if JEMPERLI passes into your breast milk. Do not breastfeed during treatment with JEMPERLI and for 4 months after your last dose.
Tell your HCP about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
The most common side effects of JEMPERLI when given with carboplatin and paclitaxel include nerve problems in your arms, hands, legs, and feet; tiredness; nausea; hair loss; joint pain; rash; constipation; diarrhea; stomach-area (abdomen) pain; shortness of breath; decreased appetite; urinary tract infections; vomiting.
The most common side effects of JEMPERLI when used alone include tiredness and weakness, low red blood cell count (anemia), diarrhea, nausea, constipation, vomiting.
These are not all of the possible side effects of JEMPERLI. Call your doctor for medical advice about side effects.
You are encouraged to report negative side effects of prescription drugs to the FDA by calling 1-800-FDA-1088 or visiting www.fda.gov/medwatch.
Please see full Prescribing Information, including Medication Guide for patients.
Trademarks are owned by or licensed to the GSK group of companies.
©2024 GSK or licensor.
PMUS-DSTCOCO240006 December 2024
Produced in USA.









