When it comes to detecting breast cancer, no test is more powerful than magnetic resonance imaging (MRI). It outperforms the latest 3D mammogram and breast ultrasound, yet few women in the U.S. had access to this screening technology until recently. Luckily, there’s a new screening method that takes less time, costs less, and has the potential to save so many lives.
A mammogram is the gold standard test for breast cancer screening, which is why you can get one almost anywhere in the country — including in a mobile van. It’s the only test proven to improve women’s survival from this deadly disease, which kills more than 40,000 women each year in our country..
The issue is that women who have dense breast tissue — nearly half of all women aged 40 and over — are at higher risk for breast cancer, and they’re more likely to have their cancer missed on a mammogram. Sadly, a late diagnosis can mean the difference between life and death. Now that legislation mandates that women be notified about their breast density in much (and soon all) of the U.S., more women are seeking additional screening after a reportedly “normal” mammogram.
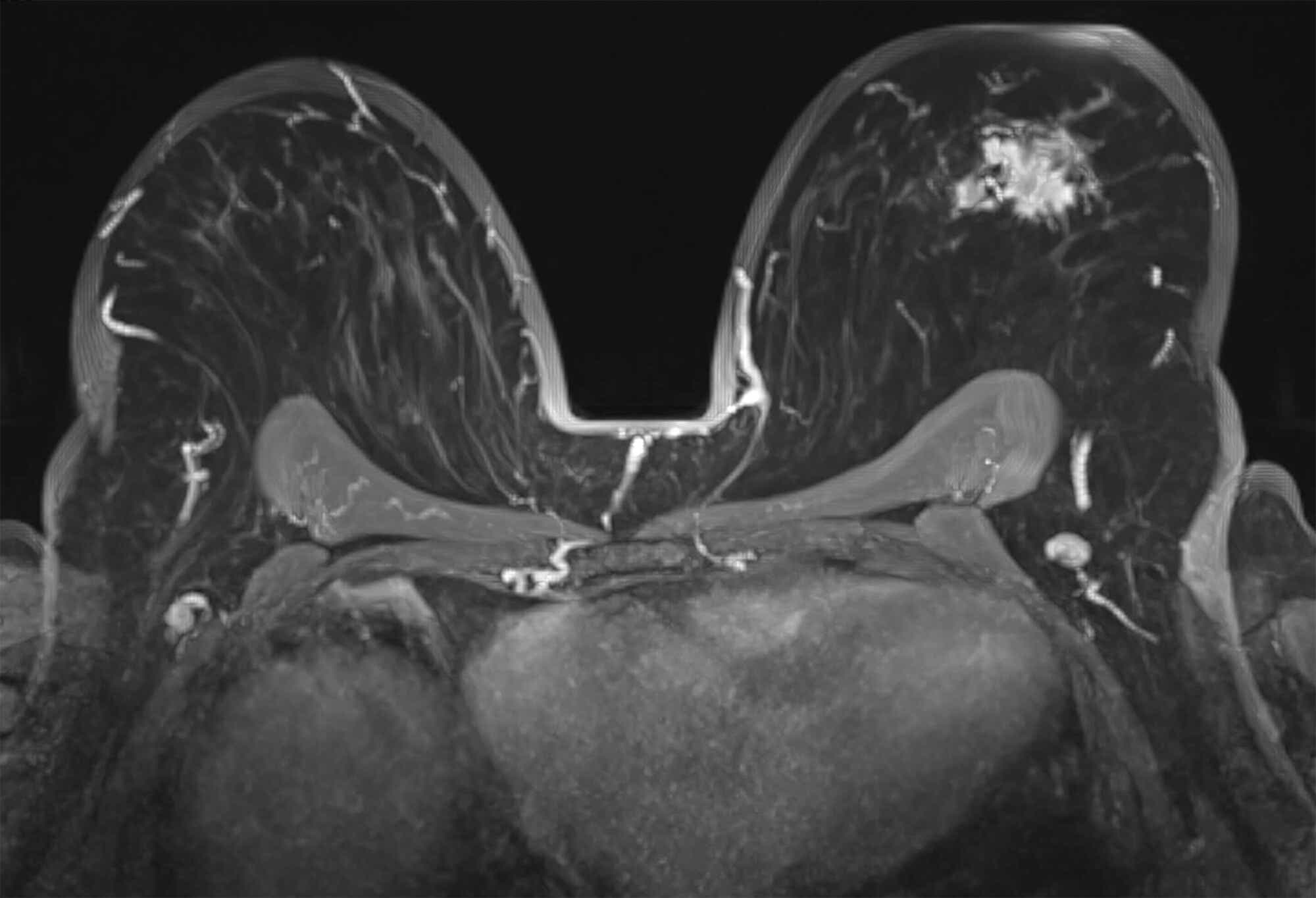
Breast MRI is the most sensitive test for early detection of breast cancer. It uses a strong magnetic field and radio waves to produce detailed pictures of the breast. Like ultrasound, MRI doesn’t use radiation (x-rays) and isn’t limited by dense breast tissue. But, unlike ultrasound, MRI uses dye injected into the bloodstream to highlight blood flow in the breast. That’s what makes it possible to find many early cancers not seen on a mammogram or ultrasound. If we screened 1,000 women after a “normal” mammogram, we would find 3-4 missed cancers with breast ultrasound and 15-18 missed cancers with breast MRI — significantly more accurate. Breast MRI is also particularly good at detecting the more aggressive types of breast cancer, which would cut a woman’s life short.
So, why isn’t everyone getting an MRI? Until recently, MRI was reserved for high-risk women with a strong family history or genetic mutation, which constitutes only 15% of newly diagnosed breast cancers each year. That’s because traditional MRIs are very expensive, and the exam can take up to an hour to perform, which is difficult for many women to get through. Also, the large magnets needed for MRI examinations aren’t available everywhere in the U.S., especially in rural areas.
However, a new breast MRI technique called “fast MRI,” which was originally piloted in Germany, has cut the MRI time down to less than 10 minutes in the scanner. The cost of a fast MRI is similar to a breast ultrasound at many centers. Most importantly, this shortened exam is as excellent at detecting cancer as a traditional breast MRI.
After the impressive results of a multi-center trial in the U.S., fast MRI is quickly being adopted across the country. They’re offered under lots of different names — abbreviated, fast, turbo, accelerated, or ultrafast — but, by any name, this test is a game changer when it comes to early detection of breast cancer. Fast MRI offers better outcomes, and a better experience for radiologists, patients, and healthcare providers alike.
Of course, all screening tests have false positives, and fast MRI is no exception. But the number of false alarms seen on MRI is similar to that of traditional mammograms. And while most insurance companies currently don’t cover the cost of fast MRIs, they’re typically offered at a flat fee (assuming you’re opting to self-pay) that’s significantly less than a traditional MRI. New research is also helping to change the conversation and might convince insurers to expand their coverage in the future.
The bottom line? Fast Breast MRI is a promising new test: It uses the most sensitive technology available, and overcomes the limitations of cost and time. It’s particularly good for women who have dense breast tissue who might otherwise have false-negative tests. Given its superior cancer detection, a fast MRI every other year in women with dense breasts could be more lifesaving and cost-effective than an annual ultrasound. Could MRI be performed as a stand-alone test, allowing women to skip their other screenings? We’re not there yet — it’s still seen as a supplemental test that shouldn’t replace your yearly mammograms. But this test has tremendous potential to change the future of breast cancer screening for the better.
Annie Brown, MD is a UC Health Breast Radiologist and Associate Professor at University of Cincinnati College of Medicine in Cincinnati, Ohio; she co-wrote Ohio House Bill 371 to improve breast density letters and expand screening coverage to include 3D mammography for all women and supplemental screening for women with dense breasts, which became state law in September 2022. Follow her on Twitter at @AnnBrownMD









