Not long ago, I went on TikTok and typed in the name of a new weight-loss drug that’s still in clinical trials and not yet approved for clinical care. I’m an obesity medicine specialist and have been researching weight management for 20 years, and I can’t get this medication for my patients yet. So I was surprised to see videos of people injecting it, swapping dosing tips, and pointing followers to places where they could “get it cheaper” through messaging apps like WhatsApp or Telegram. A physician colleague told me he’d already seen a patient who bought an experimental drug called retatrutide from an online seller. (It didn’t work for him and was probably fake.)
There is growing excitement and publicity about both the current and new obesity care medications, often called incretin mimetics or “GLP-1s” after one of the main hormones they mimic. These medications help people lose weight and control blood sugar by regulating appetite and decreasing “food noise” (those obsessive food thoughts), slowing digestion, and helping the pancreas release insulin to lower blood sugar.
It's an exciting time to practice obesity medicine, and many of my patients have had transformative outcomes because of these medicines. They've also changed the conversation around obesity, which has historically been highly stigmatized and seen as a character flaw. More people now recognize that obesity is a chronic disease that is as heritable as height.
But there's a dark side to this progress.
GLP-1 medications are also fueling our obsession with thinness and the desire to live forever. Models are using them to get even skinnier, and companies that seem legitimate are now advertising “microdosing” plans and “longevity” packages, on top of weight loss. New medications that have not yet been fully tested or FDA-approved are being sold directly to consumers “for research purposes only,” to hide the fact that people are experimenting on themselves without medical oversight. It’s no wonder so many people feel confused and overwhelmed.
If you’re using or planning to use GLP-1–type medications, my goal is to help you ensure you're getting the right medication, for the right reason, from the right source, and with the right expectations.
The right drug: not every weight-loss shot is the same
Right now in the U.S., the main injectable medications approved by the FDA for chronic weight management are liraglutide (Saxenda), semaglutide (Wegovy), and tirzepatide (Zepbound). A high-dose oral form of semaglutide for obesity is also on the way.
These medications are approved for adults with obesity (a BMI over 30), or a BMI over 27 plus a weight-related condition like high blood pressure, high cholesterol, or diabetes. Used properly, they can help people lose 10 to 20 percent (or more) of their body weight and improve metabolic and heart health.
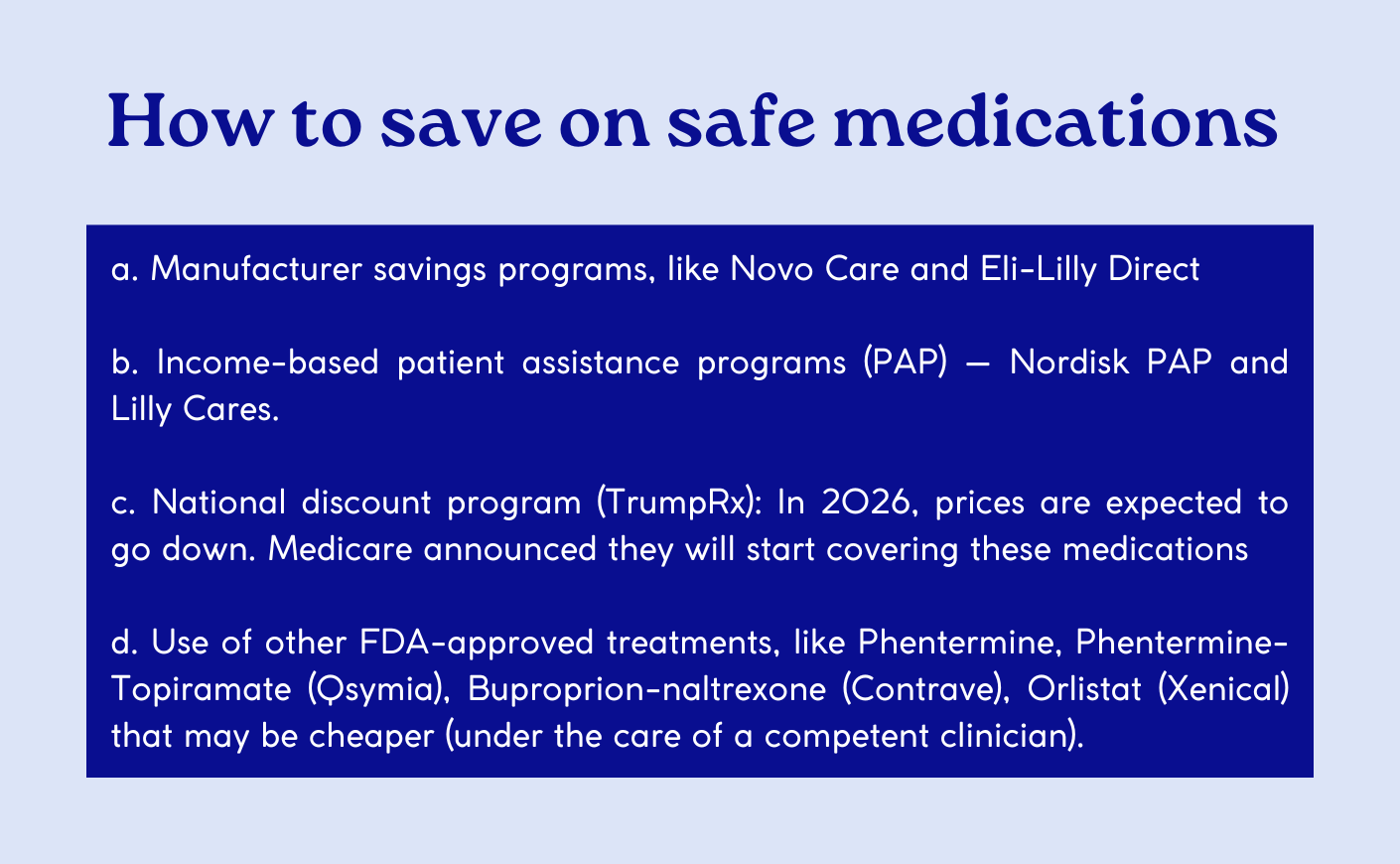
Because these medications are expensive and often not covered by insurance, many companies are now selling compounded versions at a lower price.
But compounded drugs do not go through the same FDA approval process as brand-name products, and the standards for ingredients and manufacturing are less tightly regulated. Recent reports have linked off-brand compounded semaglutide and tirzepatide to serious side effects, including hospitalizations and deaths in the U.S.
Even more concerning are drugs that are still in clinical trials (like retatrutide, cagrilintide, and others) being sold directly to consumers. These often appear as “research” peptides online, with vague product names and tiny print that reads “not for human use” or “for research only,” even though dosing instructions are provided.
If the name on your pen or vial doesn’t match an FDA-approved product, or you can’t find it on a reputable medical or regulatory site, that’s a red flag.
The right indication: are these drugs right for you?
These medications are meant to treat obesity as a chronic disease — not so you can fit into the pair of Levi's you had in high school. Like any medication, they have side effects and risks. For people with obesity and related health problems, the benefits often outweigh those risks. But it's not yet clear if that's true for healthy people using them for cosmetic reasons.
Before prescribing a GLP-1, a clinician should take a careful medical history and ideally do a physical exam to determine if the medication is a good fit for you. The clinician should ask about your current medications, what you've previously tried to lose weight, and obtain a complete diet history. They should also make sure you don't have a have a history of pancreatitis, gallbladder disease, severe reflux, or thyroid cancer.
Importantly, a clinician should also ask about your mental health before prescribing a GLP-1. If you have a history of disordered eating, depression, or suicidal thoughts, you may need to hold off entirely— or be extra careful by making sure you receive psychological support throughout the process.
I recently had an experience in which a company tried to send me tirzepatide only by having me fill out a brief online questionnaire, and without connecting me to a provider. This is dangerous, and I worry that people will get hurt by the many bad actors willing to put profits above safety.
The right source: why FDA approval and supply chains matter
The FDA requires companies to spend decades studying medications to ensure that they are safe and that they work. However, FDA approval doesn’t mean a drug is risk-free. It means:
- The medication has been studied in thousands of people in controlled trials.
- We have good data that it works for a specific condition at specific doses.
- Common and/or serious side effects are known and can be monitored
- Every batch must meet strict purity and quality standards.
After a drug's approval, the FDA continues to monitor safety and can require new warnings or even pull a medication from the market if serious problems emerge. By contrast, with compounded or gray-market peptide products, it’s much harder to know if the molecule is exactly what it claims to be, if the dose is correct, whether the vial is sterile, or whether there are contaminants like heavy metals or bacteria present — or if it's even a different drug altogether.
Before prescribing a GLP-1, a clinician should take a careful medical history and ideally do a physical exam to determine if the medication is a good fit for you.
Even some mainstream brands are now selling non-FDA-approved versions of these medications for unapproved indications or dosing. You may have seen “microdosing” of GLP-1s advertised with promises of fewer side effects and better “longevity,” though there's no clear scientific definition of microdosing, and we don’t yet have data to know if these medications prolong life (except for people with known cardiovascular disease).
The right expectations: GLP-1s are long-term tools, not a cure or a shortcut
Obesity is a chronic, relapsing disease. It's driven by a complex mix of genetics, biology, environment, and social factors. Many people with obesity are already eating carefully and moving their bodies; it isn't simply a matter of willpower.
Before starting a patient on a GLP-1 medication, I emphasize that these are long-term medications to treat the chronic disease of obesity and prevent future complications. They aren't a cure, and most people regain weight when they stop them. Nutrition, movement, sleep, mental health, and social support still matter. I make sure that patients are supported by a dietician or a formal program (like MOVE!) that helps them make healthy choices.
If you're interested in long-term weight management, here is one place where you can
find a reputable provider. If these medications aren't covered by your insurance, or if you can't afford them, your healthcare team can help you find options: just see the box below.
GLP-1 medications are tools to help people with obesity live healthier lives. As we learn
more about these medications and as new ones become available, they'll become cheaper and more accessible. We'll also learn more about new uses for these drugs. In the meantime, please make sure you receive the quality medical care you deserve — and that you're getting any medications from safe sources.
Dr. Melanie Jay, MD, MS, is a professor of medicine and population health at NYU Langone Health and a physician investigator specializing in obesity. Her research focuses on improving the treatment of obesity in medical settings and addressing weight stigma.