Breast cancer: We’re all familiar with it. You’ve seen the ribbons, or crowds of people in pink walking for a cure, or even know someone — or are someone — who has been diagnosed with the disease. But not all breast cancers are the same, and treatments will differ depending on several factors. So how do you know what signs to look out for, or how you’ll be treated if you are diagnosed?
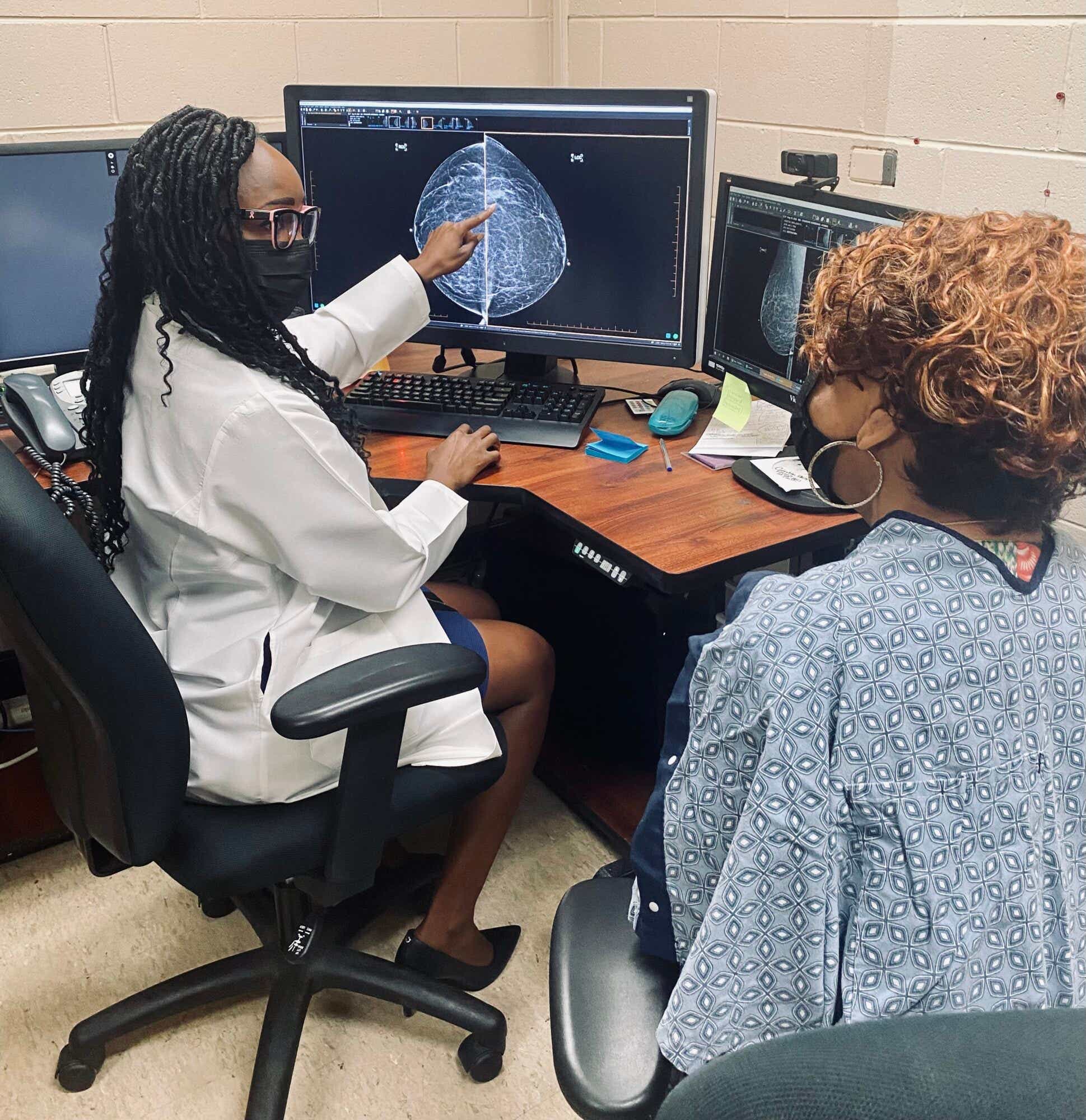
In honor of Breast Cancer Awareness Month, we asked Arlene Richardson, MD, to answer some of your most frequently asked questions about the disease. Dr. Richardson, a radiologist at Jackson Park Hospital in Chicago and a program director at RAD-AID International, has devoted her career to helping underserved women gain much-needed access to medical imaging like mammography.
Some of the info that Dr. Richardson’s shared with us about breast cancer might surprise you. (Did you know that not every breast cancer patient needs chemotherapy?) But hopefully all of it will arm you with a better understanding of the disease.
As always, your best bet in beating this insidious malignancy is through early detection. So talk with your doctor in your 20s about your risk profile for breast cancer, and don’t forget to get a mammogram annually once you turn 40.
KCM: What do the different stages of breast cancer mean, in terms of prognosis?
Dr. Richardson: Stages are just a way of describing how extensive the breast cancer is. The stage is determined by factors like the size of the tumor and how far the cancer has spread. If it has spread to the lymph nodes or to distant parts of the body, you’ll probably be diagnosed with a later stage. The lower the stage, the better the prognosis — there's a very high survival rate if you catch it at stage zero or stage one. However, the more advanced it is the more difficult it is to treat, which makes the risk of death higher. That’s why early detection is key.
Can breast cancer impact women differently depending on their race?
Yes. Race and ethnicity can impact breast cancer, particularly when it comes to things like testing, cultural perspectives on health, cancer education, and quality of and access to care. Race is often linked to socioeconomic status, so people of color may get a lower quality of care across the continuum of their health, not just breast health. Additionally, Black women have been shown to have increased breast density, which is likely genetic. And increased breast density has been linked to an increased risk of breast cancer. But in general, the guidelines for screening are the same: If you’re at average risk, you should start screening at age 40, regardless of your race.
What is breast density?
A breast is composed of fatty tissue and glandular tissue. The more glandular tissue you have, the denser your breasts. But here’s the issue: Glandular tissue is white, and so is cancer. So if you have denser breasts, cancer can be typically harder to detect in a traditional mammogram. Regardless of how cancer may present on a mammogram, women with dense breasts are more likely to develop breast cancer in general. You can’t self-assess breast density — it’s something you won’t know until you have your first mammogram. If you have dense breasts, you may qualify for additional screening, like an ultrasound or MRI.
Does it matter whether I get a 2D or a 3D mammogram?
3D mammography has been proven to be more effective in finding cancer in women with dense breasts. Say you're taking a photo and there are two people in the frame: If one of them is bigger than the other and the smaller person is behind the bigger person, you’ll only see the person in front. Think of the person in the front as dense breast tissue, and the smaller person as an abnormality that could be cancer. A 2D mammogram is like a picture — when you've got a lot of dense tissue, you can't see what’s behind it. A 3D mammogram is more like a movie: You can move past the dense breast tissue and go behind it to see the smaller mass.
If you have the option to get a 3D mammogram, you should. In addition to providing a more comprehensive picture, it decreases recall rates. That’s the term for when a doctor asks you to come back in after your mammogram for additional screening — and it’s bound to give any woman anxiety, even though more often than not, it turns out to be nothing. A 2D mammogram is still great and you should get screened regardless of the technology available at your doctor’s office, but when you call to schedule your appointment, you can ask about what’s available.
Does insurance cover 3D mammography?
Medicare and Medicaid in some states cover 3D mammograms, and most private insurers follow Medicare policy coverage. If you’re concerned, check with your insurance company before getting your mammogram.
If you don’t have insurance, check with your state health department to see what resources are available to you. During Breast Cancer Awareness Month, there are increased campaigns to encourage women to get screened and direct them toward screening services, and many organizations also provide free or discounted mammograms and cervical cancer screening throughout the year. There are also federally qualified health centers and free clinics that can either provide screenings or refer you to somewhere that offers them.
If I’m diagnosed with breast cancer, will I need both chemo and radiation therapy? What’s the difference between the two?
If you catch (the disease) early enough, you might not need either. Early stage breast cancer can be treated with a lumpectomy and sometimes radiation. Even if you have an advanced cancer, if it is HR positive, meaning it has hormone receptors, you might just be treated with hormone therapy.
Chemotherapy is usually IV therapy that is systemic, meaning it goes through your entire body. It’s meant to treat disease that might be somewhere in your body other than your breasts, but hasn’t been detected yet. Radiation therapy is targeted to treat a small area, usually in the breast or armpit area where the lymph nodes are. Whether you’ll need both chemo and radiation really depends on what type of cancer you’re dealing with.
Most of us became aware of the BRCA gene when Angelina Jolie announced in 2013 that she had gotten a preventive double mastectomy because she was carrying it. What is the BRCA gene?
It is basically an inherited mutation that increases the risk of many cancers, including breast and ovarian cancers. Women who carry the gene have a very high likelihood of getting breast or ovarian cancer, and possibly other cancers, depending on the mutation. Women who carry the gene will usually get screened earlier than women at average risk of cancer, since the mutation can cause cancer to develop earlier and can be more aggressive.
How do I know if I have the BRCA gene?
Since it's inherited, there will be a strong family history of breast cancer, because someone in your family also has the mutation. Usually the mutation is found after a breast cancer diagnosis, so if a mother with breast cancer tests positive for the BRCA gene, her daughter should also get tested. Women who are at average risk of cancer usually won’t be tested for the gene.
If I have the BRCA gene, does it mean I will definitely get breast cancer?
You won’t definitely get cancer, but your lifetime risk increases to 50 to 80 percent by age 70. That’s why some women who have the gene elect to get a preventive mastectomy.
Regardless of whether you’ve got a family history of it, one in eight women will be diagnosed with breast cancer in their lifetime. The earlier it’s detected, the higher the survival rate. And it bears repeating that if you’re 40 years old or older, you should get a mammogram every year — it could save your life.









